In the realm of medical conditions, hiatal hernias may not be as widely recognized as some other ailments, but they can significantly affect one’s quality of life. Whether you’ve recently been diagnosed with a hiatal hernia or are simply curious about this condition, understanding when surgery becomes necessary is a crucial aspect of managing it effectively.
Hiatal hernias occur when a portion of the stomach pushes through the diaphragm and into the chest cavity. While smaller hernias may not cause significant discomfort or complications, larger ones can lead to a range of symptoms and health issues. In this article, we will delve into the world of hiatal hernias and explore the pivotal question: What size hiatal hernia needs surgery?
By embarking on this informative journey, you’ll gain valuable insights into the types of hiatal hernias, the symptoms they can produce, diagnostic methods, and the spectrum of treatment options available. Most importantly, you’ll uncover the significance of hernia size in determining whether surgery is the best course of action.
What is Hiatal Hernia?
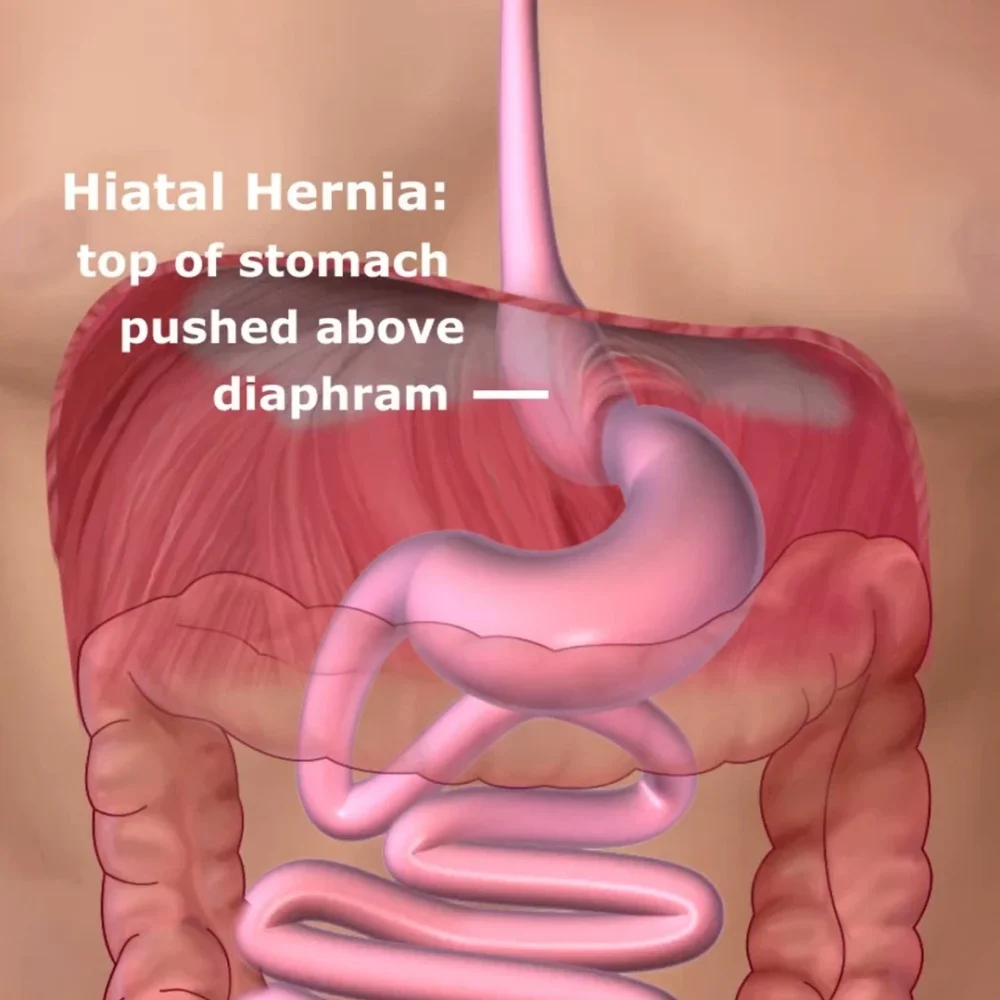
A hiatal hernia is a medical condition that occurs when a portion of the stomach protrudes through the diaphragm and into the chest cavity. To understand this condition better, it’s essential to know that the diaphragm is a muscular sheet that separates the chest cavity from the abdominal cavity and plays a crucial role in breathing. Normally, the esophagus passes through an opening in the diaphragm, known as the hiatus, and connects to the stomach in the abdominal cavity.
However, in the case of a hiatal hernia, the upper part of the stomach or sometimes other abdominal organs can push up through this opening into the chest area. Hiatal hernias are categorized into two main types: sliding and Paraesophageal, each with its characteristics and potential complications. While smaller hernias may be asymptomatic or cause mild discomfort, larger ones can lead to a variety of symptoms, making it important to understand the condition and its implications for one’s health.
Types of Hiatal Hernias
Hiatal hernias come in two main types: sliding hernias and Paraesophageal hernias.
#1. Sliding Hiatal Hernias:
Sliding hernias are the most common type. In this condition, the junction of the esophagus and stomach and a portion of the stomach itself slides up into the chest through the diaphragmatic hiatus (the opening in the diaphragm). These hernias tend to move in and out of the chest with changes in body position and swallowing. Sliding hernias are often associated with symptoms like acid reflux and heartburn.
#2. Paraesophageal Hiatal Hernias:
Paraesophageal hernias are less common but potentially more serious. In this type, a portion of the stomach pushes up through the diaphragmatic hiatus beside the esophagus and stays there. While the esophagus remains in its normal position, the stomach sits next to it in the chest. These hernias can be larger and carry a risk of complications, such as the stomach becoming trapped or twisted, which can obstruct blood flow and require surgical intervention.
What size hiatal hernia needs surgery
The decision to perform surgery for a hiatal hernia is not solely based on its size but rather a combination of factors. Generally, smaller hiatal hernias may not require surgery if they are not causing significant symptoms or complications. It’s important to note that the size of the hernia alone does not always correlate with the severity of symptoms.
However, there are specific indications for surgical intervention in hiatal hernias, which may include:
Symptoms and Complications
Symptoms and complications associated with hiatal hernias are essential aspects to understand for those affected by this condition. Let’s delve into these two categories:
| Symptoms | Complications |
|---|---|
| Heartburn and Acid Reflux: A common symptom characterized by a burning sensation in the chest or throat due to stomach acid flowing back into the esophagus. | Strangulation: This is a rare but serious complication where part of the stomach becomes trapped in the hernia, potentially leading to reduced blood supply and tissue damage. |
| Regurgitation: The involuntary return of stomach contents into the mouth, often accompanied by a sour or bitter taste. | Volvulus: Twisting of the stomach within the hernia, which can obstruct the passage of food and blood flow. |
| Difficulty Swallowing: Some individuals may experience a feeling of food getting stuck in the throat or chest when swallowing. | Ulcers and Bleeding: Chronic irritation from acid reflux can lead to the development of ulcers in the esophagus, which may bleed. |
| Chest Pain: Hiatal hernias can sometimes cause chest discomfort or pain, which can be mistaken for heart-related issues. | Anemia: Prolonged bleeding from esophageal ulcers can result in anemia characterized by a deficiency of red blood cells. |
| Belching and Hiccups: Frequent burping or hiccups, especially after meals. | Barrett’s Esophagus: Long-term exposure to stomach acid can cause changes in the lining of the esophagus, increasing the risk of esophageal cancer. |
| Shortness of Breath: Occurs when the hernia puts pressure on the diaphragm, making it difficult to breathe, particularly when lying down. |
Diagnostic Methods for Hiatal Hernias
Diagnostic methods for hiatal hernias are procedures that help doctors identify and evaluate the presence and severity of a hiatal hernia, which is a condition where part of the stomach bulges through the diaphragm into the chest cavity. Some of the common diagnostic methods for hiatal hernias are:
- Medical History and Physical Examination: The first step is a thorough review of the patient’s medical history and a physical examination to identify symptoms and assess overall health.
- Barium Swallow Radiography: This imaging test involves swallowing a contrast material (barium) followed by X-rays. It allows healthcare providers to visualize the esophagus and stomach, highlighting the presence and size of the hernia.
- Upper Endoscopy (Esophagogastroduodenoscopy or EGD): This procedure involves passing a thin, flexible tube with a camera (endoscope) down the throat to view the esophagus and stomach directly. It allows for a detailed examination of the hernia, any associated damage to the esophagus, and the presence of other conditions like Barrett’s esophagus.
- Esophageal Manometry: This test measures the pressure and muscle contractions in the esophagus, helping to assess the functioning of the lower esophageal sphincter (LES) and detect conditions like gastroesophageal reflux disease (GERD).
- pH Monitoring: This test involves placing a pH sensor in the esophagus to monitor acid levels over 24 hours. It helps determine the extent of acid reflux and its correlation with symptoms.
- CT Scan or MRI: In some cases, especially when complications like strangulation are suspected, computed tomography (CT) scans or magnetic resonance imaging (MRI) may be ordered to provide detailed images of the hiatal hernia and surrounding structures.
- Electrocardiogram (ECG): Given that hiatal hernia symptoms can mimic heart-related issues, an ECG may be performed to rule out any cardiac problems and ensure an accurate diagnosis.
Conservative Treatment Options
Conservative treatment options for hiatal hernias primarily focus on managing symptoms and reducing the frequency of acid reflux without surgical intervention. These approaches are often recommended for smaller hernias or cases where surgery is not immediately necessary. Lifestyle modifications play a significant role and may include dietary changes, such as avoiding acidic or spicy foods, reducing portion sizes, and eating smaller, more frequent meals.
Elevating the head of the bed during sleep can help prevent nighttime reflux. Over-the-counter antacids and medications like proton pump inhibitors (PPIs) or H2 blockers may be prescribed to reduce stomach acid production and alleviate heartburn. Lifestyle adjustments, such as weight loss, smoking cessation, and avoiding tight-fitting clothing, can also contribute to symptom relief.
Surgical Intervention
Surgical intervention for hiatal hernias becomes necessary in specific situations, typically when conservative treatments fail to provide relief or when the hernia presents with complications. There are several surgical approaches to address hiatal hernias:
- Laparoscopic Nissen Fundoplication: This is one of the most common procedures for hiatal hernia repair. It involves making small incisions in the abdomen and using a laparoscope to reconstruct the lower esophageal sphincter (LES) and reinforce the hiatus. This procedure helps prevent acid reflux and restores the normal anatomy of the diaphragm.
- Laparoscopic Hiatal Hernia Repair: In cases where the hernia is large and primarily involves the stomach slipping through the diaphragm, laparoscopic repair focuses on returning the stomach to its correct position and closing the hernia opening.
- Open Surgery: In some complex cases or when laparoscopic techniques are not feasible, open surgery may be performed. That involves a larger incision and direct access to the hernia for repair.
- Paraesophageal Hernia Repair: For Paraesophageal hernias, where the stomach is next to the esophagus in the chest, surgical correction is often recommended to prevent complications like strangulation or volvulus. The procedure typically involves repositioning the stomach and reinforcing the hiatus.
Life After Hiatal Hernia Surgery
Life after hiatal hernia surgery often involves a significant improvement in quality of life for individuals who previously struggled with symptoms such as acid reflux, heartburn, and difficulty swallowing. While the specific experience can vary depending on the type of surgery and individual factors, there are common aspects to consider:
- Relief from Symptoms: Surgery is typically effective in alleviating or significantly reducing symptoms associated with hiatal hernias. Patients often experience less frequent or severe acid reflux and heartburn.
- Dietary Adjustments: After surgery, dietary changes may be necessary, particularly in the immediate postoperative period. Patients may need to start with a soft or liquid diet and gradually transition to regular foods. It’s important to follow the dietary guidelines provided by the healthcare team.
- Activity Levels: Most patients can resume light activities and daily routines relatively soon after surgery. However, strenuous activities and heavy lifting should be avoided during the initial recovery phase, as advised by the surgeon.
- Follow-Up Care: Regular follow-up appointments with healthcare providers are essential to monitor progress and address any concerns. These appointments help ensure that the surgical site is healing properly and that the patient is adjusting well to life after surgery.
- Lifestyle Choices: Maintaining a healthy lifestyle is crucial to prevent the recurrence of hiatal hernias. That includes maintaining a balanced diet, practicing portion control, avoiding trigger foods, and maintaining a healthy weight. Quitting smoking and managing stress can also contribute to long-term success.
FAQs
Conclusion
Hiatal hernias can significantly impact one’s health and quality of life. Understanding their types, symptoms, diagnostic methods, and treatment options, including surgery, is essential for informed decision-making and effective management. Whether opting for surgical intervention or conservative approaches, the goal is to alleviate symptoms and prevent complications, ultimately leading to a better quality of life for individuals dealing with hiatal hernias.

Beth is Cloudmineinc’s senior health editor and a certified personal trainer. She has over 10 years experience as a science journalist and is the author of two books. She deadlifts over 315 lbs.